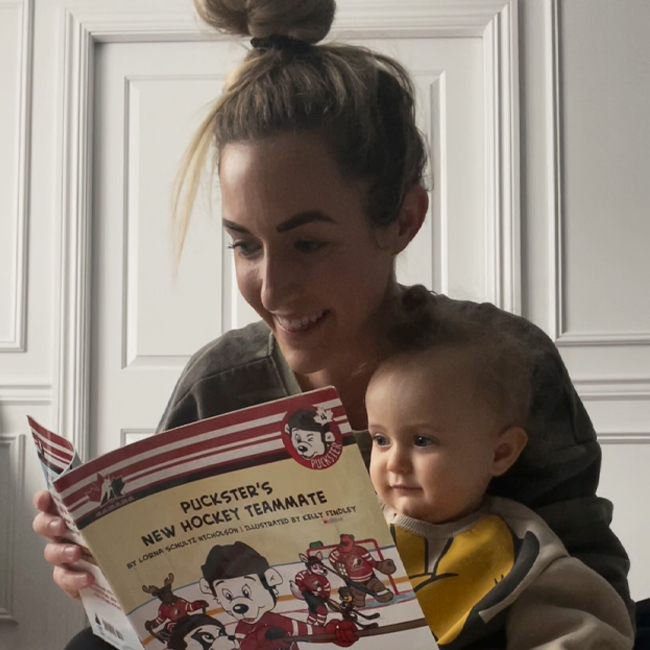
Maybe it’s the music teacher in me, or maybe it’s just the fact that I like to talk (and listen) and read, but speech is something that fascinates me. I once went to a seminar with the author of The Enchanted Hour and learned all about how beneficial it is to read out loud to people of all ages. It really opened by eyes to a fantastic way to introduce speech. When I was pregnant, I would read my books out loud, for an extra way for my baby to hear my voice, and as soon as she was born, I kept that habit up. I still read my books out loud to her, along with her books. I personally feel it’s such a beautiful way to interact with my daughter, as well as introduce her to many words that I may not use in my everyday speech. Alongside that, I’ve introduced baby sign language, to give her a way to communicate with me, as babies gross motor skills develop before their fine motor skills, one fine motor skill being speech. Currently my daughter is only about 11-months-old, and saying a few words, and doing some signs, but I loved learning from Jayme and getting to ask her all your questions as well! Hope you find some takeaways from this chat!
Hi Jayme! Thanks for spending some time talking with me today and helping parents and caregivers with this topic of speech! Can you tell us a little about yourself, personally and professionally?
Hi Lauren! Thank you so much for asking me to be a part of this. I am a Speech Language Pathologist. I went to Hofstra University for my undergraduate and graduate degrees. I received my Master’s degree in Speech Language Pathology in 2019. As part of my graduate coursework, I interned at a local elementary school working with children from grades Kindergarten through fifth grade. I also interned at a private practice, which is where I work now. I love how everything worked out! I work with children with expressive and receptive language deficits, as well as articulation deficits from the ages of 1.5-years-old to 8-years-old. When I am not working, I have a love for health and fitness (the Peloton has become a staple during quarantine). I am also a hockey fan and love watching anything on Bravo.
I am really starting to think I need to get on this Peloton-train myself! What made you want to become a Speech Language Pathologist (SLP)?
Growing up, I always knew I wanted to work with children. I worked at day camps during the summers, babysat, and was a teacher’s aid at a school for children with developmental disabilities. I went to speech language therapy as a child and watched my siblings go as well, so I was always interested in the field and the science aspect of it. I was also interested in the depth of this field. You can have the opportunity to work with both children and adults. There is a misconception that SLPs only work with individuals who have a lisp or a stutter. In reality, we work on feeding, swallowing, voice disorders, fluency, speech sound disorders, expressive and receptive language deficits, and more! The list goes on!
Where should adults begin before a baby even has speech? I know there is lots of research about the use of open cups and straw cups. Also, I know there is research now showing we shouldn’t be offering the 360-cup for development. So, all that being said, can you share some knowledge about what us parents and caregivers can do to help prepare for the development of our baby’s speech?
I will provide some helpful language facilitating techniques later on, including providing age-appropriate toys, singing, using simple signs along with the verbalizations (ie. “more,” “all done,” “give me”).
In terms of cup use, the 360-cup is not recommended. When children use this cup, they are using excessive jaw movements to drink the liquid out of the cup. Therefore, it is important for the child to first drink from an open cup and then eventually a straw cup.
Is there always a concern with a tongue tie, and how should you know when/if you should have it addressed?
According to ASHA (2005), a tongue tie, also known as “ankyloglossia” is usually detected soon after birth. However, the effects of being tongue-tied vary across children. Tongue-ties may cause feeding problems, but it depends on the severity. According to ASHA (2005), 25% of newborns may show trouble latching during breastfeeding, whereas other children may show no early feeding problems. Problems may persist depending on the severity of the tongue-tie.
While a tongue-tie is noted soon after birth, it can be left alone unless there are feeding problems. If a child has a difficult time latching during breastfeeding with a tongue tie, then it should be clipped. In the event the frenulum needs to be clipped, it can be done by an otolaryngologist or an oral surgeon.
If you can name an age, at what age should you start to address the following challenges for a child? If you have any strategies to help them, please share!
Late Talker/Speech Delay
If a child is a late talker or speech delayed, it is never too early to get an evaluation. Later on, I’ll address how many words a child should be able to speak by each age, which are strictly estimates. I also have techniques and toys that I’ll recommend.
Stuttering
Before I get into this next topic, it is important to note that all individuals have moments when they do not speak smoothly, which are called “disfluencies.” This means that if we show disfluencies, this does not necessarily mean that we stutter. There are also language-based disfluencies, which happen in children who have language deficits. People who stutter may have more disfluencies, such as repeating parts of words (repetitions), a hard time getting a word out (blocks), and hold out a sound for extensive time (prolongations). Stuttering may also include tension and negative emotions towards talking.
Stuttering occurs in 2-5% of children. Some children recover with and without treatment. There is an idea of “natural recovery, which states that one will recover without formal treatment, and it is estimated that 60-80% of individuals will. The younger the child is, the better chance he or she has of recovery. Therefore, the probability of recovery decreases with age. If one waits too long to address stuttering, the treatment may not be effective. Research also shows that more girls than boys recover from stuttering, and one is more likely to recover if he or she has a relative who recovered.
If you think your child stutters, it is important to intervene early. According to ASHA, if the child starts to stutter more often, the child tenses up, the child avoids talking, there is a family history, the child still stutters after 3.5-years-old, or the stutter has lasted from 6 to 12 months of time or more, intervention is necessary.
Some helpful tips that a parent can implement is environmental changes. It is important for the parent to slow down their rate of speech and to tell the child to slow down as well. Increase the pauses, decrease the rate of speech, and leave extra spaces. This will help decrease the child’s rate of speech, which would help decrease the disfluencies. It is also important to reduce the demands on the child. Avoid asking your child open-ended questions, putting him or her on the spot, and instead give the child choices.
Lisp
A lisp can be frontal (meaning the tongue sticks out between the front teeth) or lateral (when air escapes over the sides of the tongue). Lisps are very common in children. If the child continues to have a lisp by 7-years-old, intervention is necessary, as the lisp will be more difficult to correct. If the child is receiving speech therapy services, have the child look in the mirror and have them make their “snake sound” by putting their tongue behind their teeth and saying “s.” Visual cues are important!
Letters and Sounds
Speech pathologists also focus on language and literacy. Children learn language from the day they are born. Early speech and language development promote the development of literacy, which is referred to as the emergent literacy stage. According to ASHA, this stage begins at birth and continues throughout the preschool years. Children begin to interact with print (books) daily. It is important for children to learn letters and the sounds that letters make early on. Children who have phonological deficits are more susceptible to phonological awareness difficulties, which will impact their ability to learn how to read.
What are some of the last sounds developed by a child? Many people say “th” words are a struggle, and often come out as “f” – what can adults do to support this development along?
The last sounds developed by a child are /r/, /zh/, and voiced/voiceless /th/. When I refer to voiced sounds or voiceless sounds, I am simply talking about the vocal folds moving. When your vocal folds vibrate, the sound is voiced. If you say the word “thanks” and put your fingers over your throat, you should not feel your throat buzz. Therefore, the /th/ sound here is voiceless. Now if you say the word “that” and put your fingers over your throat, you should feel vibration of your vocal folds. When working on /th/, I always start with the voiceless /th/ and I start with the sound in the beginning of the word.
If the /th/ sound is not acquired by 7-years-old, I would recommend getting the child evaluated for speech. This can be done privately through an agency, private practice, or within the school district.
When working with any speech sound, you want to give it a “nickname.” I call the /th/ sound the “tongue-sandwich” sound. I explain this by telling the child we put bite on our tongue (just a little bit), and blow. It also helps tremendously working on these sounds by using a mirror; this technique gives the child visual supports. If the child is stimulable [can imitate] for this sound (or any sound), the SLP should pick a few words that are part of his or her core vocabulary, and words they will have the most success with. I usually choose 5 words for the child to practice.

Coming back to this, how many words should a child know by different ages (up to 3-years-old)?
According to Lanza and Flahive (2008), children’s vocabulary grows rapidly from the time of their first word at around 12-months through first grade. Here are the approximate words by age from 12-months up until 36-months:
- 12-months: 2-6 words
- 15-months: 10 words
- 18-months: 50 words
- 24-months: 200-300 words
- 36-months: 1000 words
Vocabulary increases due to exposure, education, and a child’s life experiences. Also, it is important to understand that these are approximate ages in which children have a specific number of words. Children all develop differently, but these are the norms that are followed.
That’s really great to point out – every child is different! What is one thing parents and caregivers can do daily to support speech?
Another great question! Here are some child-directed approaches to support speech: Forced Choice, Expansion, and Parallel-Talk.
Forced Choice
Forced Choice is the idea of giving the child two choices, and this can be done at any level. For example, a parent or caregiver can hold up 2 choices of a toy, food, drink, or color and ask the child which one he or she wants. This is a great way for the child to request. When using choices, the child may request by pointing, reaching, gazing, or with words.
Expansion
Expansion is the idea of taking what the child has said and adding details, such as grammatical markers and semantic details that would make it an acceptable adult utterance. For example, if the child says, “doggy run,” you can say “The dog is running.” Super Duper has helpful handouts teaching this strategy.
Parallel-Talk
Parallel-Talk is another great technique, and I am sure many parents and caregivers use it without even realizing there is a name for it. Parallel talk is when we talk about what the child is doing. For example, if your child is cleaning up, you can say “Wow, you are cleaning up!” You are simply narrating what the child is doing.
It is also important that parents and caregivers have age-appropriate toys and games for the child. From a clinical perspective, I use wooden puzzles (ie. animal puzzles), toy food, Mr. Potato Head, stacking cups, shape sorters, and animals and a farm for the little ones. Books are also fantastic for early language exposure! One of my favorites to use includes “Brown Bear, Brown Bear.” Language can also be facilitated with songs! “Wheels on the Bus” and “Old MacDonald” are two favorites that can be sung with the use of manipulatives, gestures, and words!
What are some things you, as a SLP, or caregivers can do to help a child with Social Pragmatic Communication Disorder [defined as a diagnosis characterized by impairment in verbal and non-verbal communication for social purposes]?
SLPs and caregivers should work on social reciprocity, which is the back-and-forth flow of social interaction. It is also important to work on peer and adult interaction, imitiating conversation, turn-taking, and responding to questions.
For those interested in becoming a SLP themselves, do you have any advice – where to start, what to look into, how to prepare for the exams?
First, I would say, you are making a fantastic choice. While the road was not easy, I am very grateful that I am in this field. When looking at schools for undergraduate work, make sure that the school has an official speech program, and there are opportunities for an internship. This will help with the graduate school application process, and also help you decide whether you want to be a SLP or an audiologist (one who works with hearing and balance disorders). Also, make sure there are opportunities for you to observe a professional. While I was an undergraduate student, I observed SLPs, as well as audiologists. I had exposure to both speech pathology and audiology and decided to go with speech. It is also important to get involved with the National Student Speech and Language Hearing Association (NSSLHA) and to work hard at achieving a high GPA. Applying to graduate school is competitive, and it is important to stand out.
When looking to apply for graduate schools, make sure you look at programs that are accredited by the American Speech-Language-Hearing Association (ASHA) [or the equivalent in your area]. Most graduate schools require a GRE exam to be taken prior to application and/or an interview at the campus. On ASHA’s website, there is a list of schools, by state, that are accredited.
Once you start your graduate career, try not to be discouraged. It is an adjustment, and time management is everything! You will learn the diagnostic parts of speech language pathology (i.e. administering standardized and informal tests, interviewing parents/families/clients, conducting evaluations) and the treatment aspect (i.e. treating speech and language disorders). Do not be afraid to ask your professors or supervisors questions! It is also okay if you are unsure of what population or setting you want to work in. That is what makes our field so great! I work at a private practice with children who exhibit articulation, as well as expressive and receptive language delays. Other settings that may excite you include hospitals, schools, skilled nursing facilities, etc. Many speech language pathologists also work with individuals post-stroke, who have a traumatic brain injury, voice disorders, or even swallowing disorders.
During graduate school, there will be tons of research papers, group projects, exams, reports, and externships. During the end of graduate school, you will have to take the Praxis exam, which covers all of speech language pathology. You will know more than you think! Buy the practice book and take practice tests. Since I went to school in New York State, and in case I ever decide to work in a school, I took the Educating All Students (EAS) exam for my teaching certification. Hofstra’s Graduate Program also required me to take a comprehensive exam based on everything I learned in graduate school.
Last bit of important information, prior to graduation or post-graduation, you will look for a clinical fellowship (CF). A CF is a mentored professional experience that begins after academic work is completed and can be available in any setting. This is a 9-month experience that is a minimum of 1260 hours and 36 weeks of full-time experience. Keep in contact with your externship supervisors from graduate school or even look on Indeed for opportunities. You must complete a CF to receive your Certificate of Clinical Competence in Speech-Language Pathology (CCC-SLP). More information is available on ASHA.
Looking back to graduate school, it was an emotional rollercoaster. Make friends, have a routine, and most importantly, take care of yourself. The hardest part for me was making sure I devoted 30-45 minutes of my day to workout or decompress. Self-care is extremely important. There is also NO reason to be competitive with your peers; everyone gets accepted to graduate school for the same reason and everyone will get a job after graduation.
Wow, thanks for all that detail! I’m sure that will help those interested in becoming a Speech Language Pathologist know where to go with this career path! Is there anything else you would like to share?
I hope I helped! My answers are detailed, but the field of speech and language pathology is not black and white! I am grateful to be in this field and have the ability to impact so many lives in such a rewarding way.
Where can people follow along with you or support you?
Right now, I do not have social media focused on my work, but I am thinking about making one! For now, you can connect with me on LinkedIn, send me an email at Jaywoghin@gmail.com, or even follow me/send me a message on Instagram for the time being. I will always reply!
Thanks again, Jayme! Now, I’m off to go put all these things into practice!